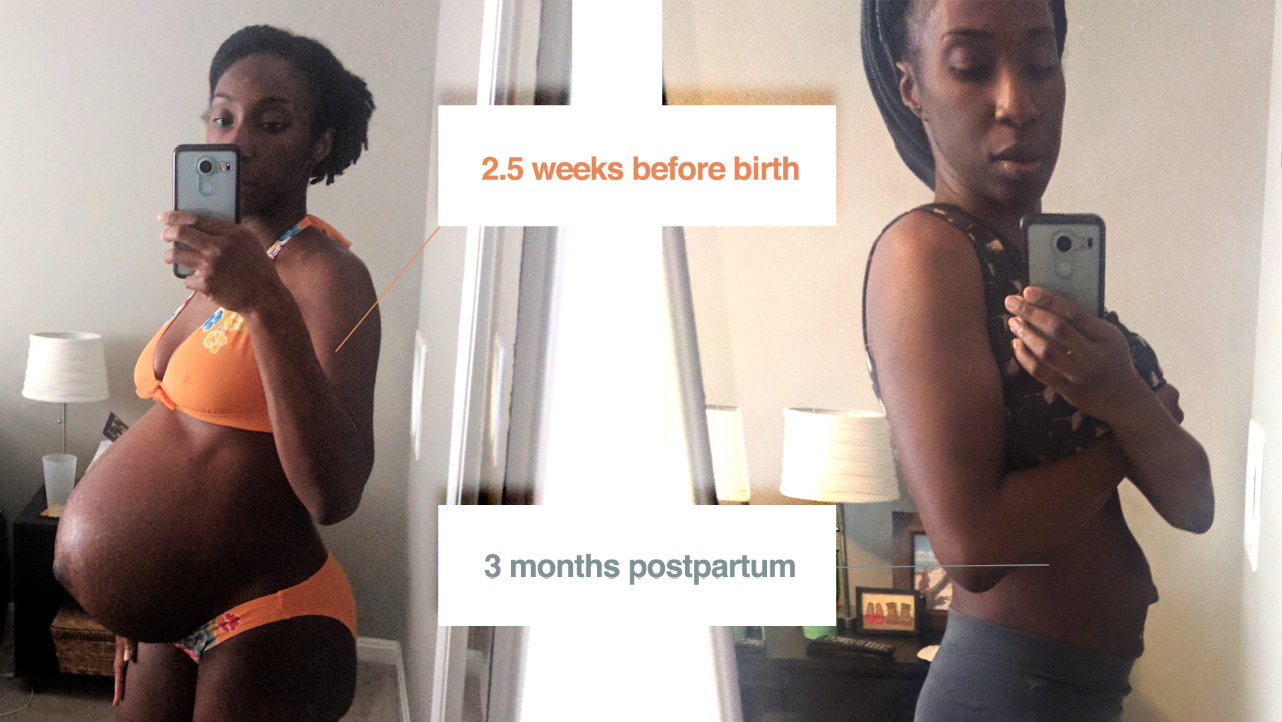
Postpartum Physical Therapy: My Diastasis Story
I’d finally started listening to my heart and body this time last year. It was February of 2019 when I finally decided to address the nagging pain in my back, the result of a strained postpartum core and abdominal separation.
Diastasis recti is the technical name for abdominal separation. The abdomen naturally separates during pregnancy to make room for your growing baby. This internal abdominal pressure can cause the linea alba (which is in between your abs) to stretch out, creating a gap between your abdominal muscles.
Some describe it as a pooch that pokes out of the middle of the stomach, often pushing your belly button back out if you were born with an outtie like me. Most women will have their “pooch” for months and sometimes years after giving birth.
At least 60 percent of women have it six weeks after giving birth, while 30 percent still have it a year after giving birth.
Source: Madame Noire
My separation was almost 3 fingers wide after I birthed Malcolm. That's how a diastasis is measured; with fingers to check for the width and depth.
I had a separation of almost 2 finger widths from my first pregnancy, something that wasn’t found until my 9-week check-up during my son’s pregnancy. My OB hadn’t checked for one and I never developed any pain or discomfort as a result, so my little belly gap went undetected. And after having Malcolm, it went from 1 ½ to 3 fingers wide.
I wanted to share my diastasis story here for a couple reasons.
1 |
Diastasis is a real part of a 4th trimester reality that can be hard enough.
I wasn’t educated about diastasis until my 2nd pregnancy. And having a tummy gap isn’t simply a vanity issue. It can cause back pain, decreased mobility and even put you at risk for developing a hernia.
The quality of postpartum life is critical to the well-being of new mothers and babies. Most new mothers will struggle with their new bodies and feel the pressure of the “snap back” culture. But we have to be gentle with our bodies. Flooding the postpartum narrative with more conversations about our real rehabilitative needs after delivery is a wonderful start.
2 |
Our postpartum bodies deserve the utmost love and adoration. That includes addressing how our bodies FEEL, not just how they look.
In the midst of a black maternal health crisis, postpartum support and recovery of the black birthing body is paramount. I am grateful that I had access to a village because far too many of us don’t. Far too many black women are trapped by barriers to care.
According to an article from the National Women’s Law Center, “…providers are also more likely to underestimate the pain of their Black patients, ignore their symptoms, or dismiss their complaints.”
Source: National Women’s Law Center
It’s more critical than ever that we listen to our bodies and address our well-being. This only makes us stronger. We need healthy bodies first for ourselves, then for our families and to be beacons in our maternal health advocacy.
May we all recognize that our post baby bodies are beautiful and worthy of tending to. Here is my story:
It started as a twinge in my lower back each time I picked up my son.
Soon it grew into a sharp, aching mess every time I got out of bed in the morning, bent down or even turned my torso.
I waited longer than I should have to address it. I knew that my core strength was completely gone after having Malcolm. I carried him high and waaaay out. Several weeks postpartum, my stomach would move like gentle waves when I laid on my back, my intestinal activity visible through weak, thin layers of connective tissue. Whenever I sat up or put even slight pressure on my core, my belly would bulge until a form of a baguette appeared, a hallmark sign of diastasis.
I endured months of nagging pain and frustration before I finally called Ann.
“Many postpartum women have little to no awareness of what pre or postpartum PT [physical therapy] is, let alone that it’s available to them.”
– Ann Udofia, PT, DPT
Our first appointment felt like a long-awaited exhale. I met Ann when she was a part of Body Connect, a DC area physical therapy practice recommended to me by one of my midwives.
Part of me felt really embarrassed to admit to her that I’d been in constant pain for so long without asking for help.
It’s a vicious cycle we find ourselves in as mothers; waiting pain out, ignoring signs of distress until we find ourselves desperate for help and any relief.
But Ann held space for me. She understood exactly what I was feeling. I quickly related to her, a black mother of two young children of her own and someone who had dealt with pelvic pain herself. I knew she wanted my pain alleviated as much as I did.
Our first appointment involved a history assessment and physical exam where she confirmed my diastasis. Ann explained that the muscles around my spine and pelvis were overcompensating for my weak core. They were carrying a load that my weak abdomen couldn’t.
And my biggest aha moment? Learning first what a psoas muscle is (pronounced SO-AS) and then understanding that IT was the real cause of my “back pain.”
“The inside of my body changed, and it was a moment when my core became extremely weak, which gave me back problems—Diastasis recti,” she said.
“It affected my abs, which affected my back. I don’t care about being skinny more than I care about being healthy.”
— Kelly Rowland, Madame Noire 2018 article
I didn’t know it then, but even fit & fabulous Kelly Rowland felt my pain.
During each visit, Ann treated my overworked muscles with patience, focus and what I knew was a true understanding of how I felt not just physically, but emotionally.
Some of the sessions were challenging for me because my muscles and tissue were so tight. I hadn’t moved my body or stretched diligently in a minute. I went from nursing, to sitting for hours on end for my work, then right to bed. “Your muscles should feel like a nice filet. Right now, your muscles are like beef jerky,” Ann explained.
The atmosphere was conducive to her work and my peace. She always played relaxing music. She always asked if the pressure was too much or too little.
Our sessions always felt like a dose of
self-care, the conversation light and familiar.
With her simple technique for proper core engagement and exercise suggestions, I was finally getting some relief. Over the course of several weeks and since seeking out physical therapy, I went from waking up in pain to improved posture, a big reduction in my pain and ways to work on my poor, beat down psoas.
A year later, my gap is down to 1.5 finger widths. I’m stronger and happier. I’m able to enjoy yoga, dance fitness and I wake up pain-free.
I often think about the women that are still suffering in silence, for many reasons, most of which involve lack of access and knowledge about postpartum physical wellness.
During our time together, Ann shared with me that I am one of a handful of black patients she has seen in her many years of practicing.
I recently asked Ann how she sees the state of postpartum PT care for black women:
L: Do you think black women face barriers to pregnancy / postpartum PT care?
ANN: Absolutely!
Prenatal or postpartum physical therapy in the US is yet to be established as a ‘standard or necessary’ component of pre/postpartum health. This is despite its effectiveness in conservatively treating common pregnancy and postpartum related issues like pelvic organ prolapse, urinary incontinence, diastasis recti and low back pain.
I do believe that the limitation is more so for women of color, particularly when institutionalized barriers exist such as lower quality maternity care for predominantly black serving hospitals or reports of black women feeling unheard or being dismissed by their providers.
L: How can these barriers could be mitigated?
ANN: I these barriers are largely institutionalized and multifactorial.
For my colleagues and fellow health care providers: It’s our responsibility to get the training needed to be culturally literate and responsive to the needs of our perinatal and postpartum African American patients.
Our patients should have an expectation that as providers, we know the risk factors that black women face that are higher compared to women of other races like pre-eclampsia, hemorrhage and cardiovascular issues.
The onus is on providers to get educated in order to provide the very best in preventative care and meet the unique needs of African American women.
As health care consumers, black women must be empowered. We have to know our risk factors and confidently explore treatment options like physical therapy for urinary incontinence or acupuncture for high blood pressure.
It’s important to speak candidly with health care providers about what we are experiencing. We have to trust our gut, seeking a 2nd or even a 3rd opinion when we get answers that are inconsistent with our experience.
I highly recommend getting connected with a community groups (online or in person) of other moms. These groups offer empowerment, education and additional resources. It can be easy to dismiss our symptoms as something that every pregnant or postpartum woman goes through. Reaching out to others in a safe space can be invaluable.
You can follow Dr. Ann and get tips and rehabilitative resources from her IG channel.